PERSONAL DETAILS:
Forenames: László
Surname: Madácsy MD, PhD, DSc
Specialty: Nuclear Medicine, Internal Medicine, Gastroenterology, Digestive endoscopy
Home Address: Toboz street 7, Sukoró, Hungary, Székesfehérvár
Postcode H-8000
Country Hungary
E-mail Address: endomabt1@gmail.com
Telephone (home): +36-22788365
Telephone (mobile): +36-704149646
Nationality: Hungarian
Gender: male
Date of Birth: 20/06/1964
Marital Status: Married

KNOWLEDGE OF LANGUAGES:
| Language | Skill (if you speak very good, please write ‘fluent’) |
|---|---|
| English | fluent International Certificate Conference (ICC), Certificate in English, 02942151051249097/1998 Frankfurt Main, Grade 1 (excellent). |
ABOUT ME:
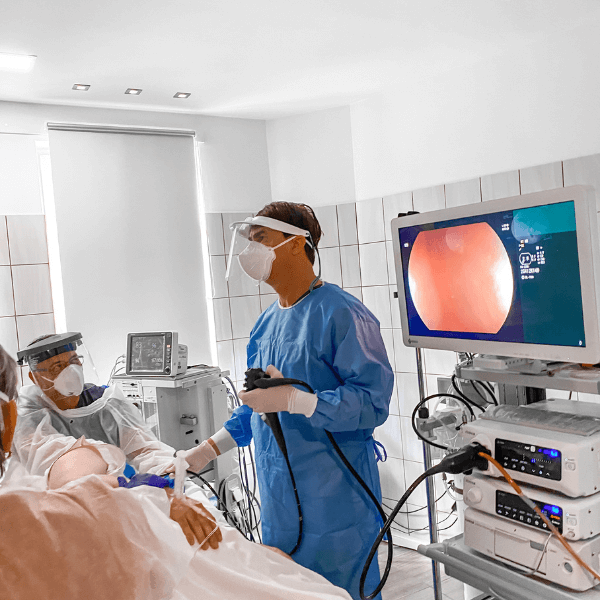
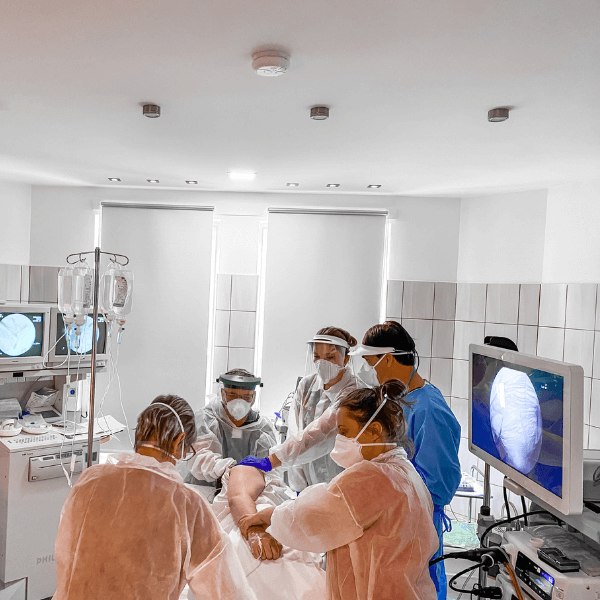
My name is László Madácsy MD, PhD, DMSc. I am a Chief Consultant Physician and Gastroenterologist and I specialised in the diagnosis and treatment of a wide variety of digestive disorders, especially functional and motility diseases, GI endoscopy, gastroscopy, colonoscopy, capsule endoscopy, EUS and ERCP. My base is the Department of Gastroenterology and Endoscopy, 2nd Department of Internal Medicine at the University of Semmelweis, an internationally-respected hospital specialising in diseases of the intestine. I’m fellow member of the European Board of Gastroenterology and Hepatology. As a board member of the Education Committee of the European Society of Gastrointestinal Endoscopy (ESGE) I made a lot of efforts in education and teaching of G.I. endoscopy. I see a lot of patients referred for endoscopy and ERCP by local GPs as well as those by specialists from Hungary and abroad whose problems are more complex and require the special skills of our multidisciplinary endoscopy team.
I have also been practicing as a medical director in our private endoscopy clinic independently since 2009 and have a well-established private gastroenterological practice based at Székesfehérvar, 60 kms far from the Liszt Ferenc Airport of the city of Budapest. Our main message here is painless endoscopy as we providing anaethesiologist controlled deep sedation or IT narcosis for all of our endoscopy patients to achieve their complete cure, respect and satisfaction. We also run services for painless colorectal and GI cancer screening with fecal occult blood tests, capsule endoscopy and PET-CT.
MEDICAL AND ACADEMIC DEGREES:
| Degree | Subject or speciality | Year |
|---|---|---|
| MD | Doctor of Medicine, University of Szeged, Hungary, Summa cum laude | 1988 |
| PhD | Clinical Sciences, University of Szeged, Hungary, Summa cum laude | 23/2001 |
| Med. Habil. (DSc) | Clinical Sciences, University of Szeged, Hungary | 6/2007 |
| Associate Professor | Associate Professor of Medicine, University of Szeged, Hungary | 23-38-2009 |
| Private Professor | Professor of Medicine, University of Szeged, Hungary | 23-8-2019 |
QUALIFICATIONS/EDUCATION:
| From (year): | To (year): | Name and location (city) of University | Subject or specialty | Level of course (diploma, degree, certificate, etc) |
|---|---|---|---|---|
| 1988 | 1993 | University of Szeged | Internal Medicine | Excellent, 1517/1993 |
| 1993 | 1995 | University of Szeged | Nuclear Medicine | Excellent, 986/1995 |
| 1995 | 1998 | University of Szeged | Gastroenterology | Excellent, 338/1998 |
| 2011 | 2012 | European Board of Gastroenterology and Hepatology | Certification of European Union of Medical Specialists (EUMS) | Excellent 1354/ 2012.12.04 |
| 2019 | 2019 | University of Szeged | License for Endoscopic Ultrasonography | Excellent 151/2019 |
ACCOMPLISHMENT OF INTERNATIONAL MEDICAL COURSES AND ELEMENTS OF TRAINING:
| Year | Name and location (city) of university | Subject or specialty | Level of course (diploma, degree, certificate, etc.) |
|---|---|---|---|
| 1997 | Semmelweis Medical University, Budapest | Ultrasonography of the abdomen | Excellent, 997/1997 |
| 1995 | University of Engineering, Budapest | Extensive training course for radiation protection | Excellent, 393-92-1995 |
| 1994 | Sophia Hospital Zwolle, The Netherlands | Third advanced post-graduate course in gastroenterology | Excellent |
| 1996-1997 | Hvidovre Hospital, University of Copenhagen, Denmark, Prof. Peter Funch-Jensen DMSc | Research Grant of the Hungarian Education Ministry, manometry, esophageal pH monitoring, antroduodenal and sphincter of Oddi manometry (ESOM) | Clinical scientific work, PhD |
| 2000-2001 | Endoscopy Unit, Surgical Gastroenterology, University of Aarhus, Denmark, Prof. Aksel Kruse DMSc | ERCP, Therapeutic-ERCP, Endoscopic SO manometry, operative endoscopy | ESGE endoscopy training course |
| 2002 | Interventional endoscopy unit, Hamburg, Germany, Prof. Nib Shohendra | Linear and radial EUS, EUS-FNA, EUS-guided pseudocyst drainage, therapeutic ERCP, mucosectomy | ESGE with Olympus Europe: Therapeutic EUS and Endoscopy |
| 2004 | Endoscopy Unit, University of Tokyo, Japan, Prof. H. Yamamoto | Double balloon enteroscopy, Endoscopic Submucosal Dissection (ESD) | ESGE with Fujifilm Europe: Endoscopy Course |
| 2014 | University of Szeged, Hungary, Prof. János Borvendég | Good Clinical Practice (GCP) | GCP course |
| 2019 | Prof. Dr. Thomas Gottwald, London, UK | EFTRD (Endoscopic full-thickness Resection) | OVESCO training course |
EMPLOYMENTS:
| From (year) | To (year) | Employer | Location (city) | Position |
|---|---|---|---|---|
| 2011 | Ongoing | Department of Gastroenterology, Bács-Kiskun Country Hospital, Kecskemét, Teaching Hospital University of Szeged | Kecskemét | Consultant |
| 2011 | Ongoing | Endo-Kapszula Private Endoscopy Center | Székesfehérvár | CEO, medical director |
Current employment description:
In 2011, I became the owner, CEO, and medical director of Endo-Kapszula Endoscopy Center in Székesfehérvár, Hungary. Our private outpatient institute is specialized to internal medicine, gastroenterology, diagnostic and operative endoscopy, radiology, computer tomography, and capsule endoscopy. We have 35 employees, 5 gastroenterologists, 2 PhD doctors, 3 endoscopic nurses, 2 CT operators, 10 general medical assistants and we perform about 4.500—5.000 endoscopic and 350 capsule endoscopic procedures in each year.
We are an approved training center of University of Pécs and University of Budapest for gastroenterology and endoscopy. Our institute is the training center of the Fujifilm Endoscopy Hungary (HUNMED) and the Ankon robotic capsule endoscopy systems in Middle Europe. We are also running PhD school in cooperation with the University of Szeged. I still give yearly lectures and classes at the University of Szeged and at the Semmelweis University for Hungarian and English medical students. As a CEO, I am responsible for the economic structure and stability, accounting and controlling, the system organization, the marketing, the medical protocols including COVID-19 defense measures, the organization and functional operation of the endoscopy and CT department facilities.
PREVIOUS EMPLOYMENT:
| From (year) | To (year) | Employer | Location (city) | Position |
|---|---|---|---|---|
| 1988 | 1990 | Department of Nuclear Medicine, University of Szeged, Hungary | Szeged | Resident |
| 1990 | 2004 | First Department of Internal Medicine, Gastroenterology, and Digestive Endoscopy University of Szeged, Hungary | Szeged | First Assistant of the Professor |
| 2004 | 2011 | First Department of Internal Medicine, Nephrology and Gastroenterology; Olympus Medical Care Hungary Endoscopy Unit | Székesfehérvár | Medical Director of the OMCH Endoscopy Unit, and Head (chief doctor) of the Gastroenterological in-hospital ward |
| 1997 | 1998 | Hvidovre Hospital Denmark | Coppenhagen | PhD student |
| 2000 | 2001 | Endoscopy Unit, Arhus University Hospital, Denmark | Aarhus | Endoscopist |
Previous employment description
After I had finished Medical University, I started to work in the Nuclear Medicine Laboratory of the University. Two years later, I moved into the First Department of Internal Medicine to complete my qualification in internal medicine in 1993. Since the year 1990, I have worked continuously as a bedside physician and wanted to be a good internist. Since the main medical profile of our university clinic was gastroenterology, I continued my education and in 1997 awarded a qualification from gastroenterology. I started to perform routine diagnostic upper GI endoscopy in 1994 and colonoscopy in 1995. I have participated in the duty call emergency system for GI bleeding patients since 1997. In 1997 I started to practice ERCP, and currently, I am one of the few well-known ERCP experts in Hungary. From 1996 to 1997, I have worked in Denmark (clinical sciences) with Peter Funch-Jensen, Aksel Kruse, Liselotte Hojgaard and Peter Matzen in Copenhagen (Hvidovre Hospital) and Aarhus (University Hospital, Endoscopic Lab.). My scientific work focused mainly on the diagnosis and therapy of postcholecystectomy syndrome and sphincter of Oddi dysfunction. In Denmark, I have learned the methodology of GI motility investigations, ERCP and endoscopic sphincter of Oddi manometry.
After I had returned to Hungary, in 2001, I successfully defended my scientific degree (PhD) titled: “New scintigraphic and manometric methods in the diagnosis of functional biliary disorders”. Later on, my diagnostic knowledge was extended by scintigraphic investigations in gastroenterology, abdominal ultrasound and endoscopic ultrasound. In the university clinic, I reached my highest position as the first assistant professor in 2002. During the last few years, from 2000, I was the primary consultant gastroenterologist in the University Intensive Care Unit of Szeged. I am a member of the International Gastro-Surgical Club, European Association of Nuclear Medicine, Leading Committee of the Hungarian Association of Gastroenterology and Endoscopy. I completed the International Certificate Conference (ICC), Certificate in English, 02942151051249097/1998 Frankfurt Main, Grade 1 (excellent). Up till now, I have given lectures at the University of Szeged for Hungarian and English classes.
In 2004 I got a leader doctor position in the Fejér-Megyei Szent György Country Hospital, to lead the First Department of Internal Medicine and Gastroenterology ward, which was consisted of 150 in hospital beds and an outpatient clinic. In the outpatient clinic, the following facilities are currently running: Olympus Medical Care Hungary (OMCH) Endoscopic Laboratory (5 investigation rooms, two gastroscopy, two colonoscopies, 1 ERCP and the endoscopic US), functional motility laboratory (24 h pH, oesophagal, gastroduodenal, and sphincter of Oddi manometry), abdominal ultrasound laboratory. In our department, we had 17 medical doctors; 9 of them have specialized in gastroenterology and endoscopy. I was a medical director of the OMCH Endoscopy Unit, where we perform about 9750 endoscopic procedures per year, including upper GI endoscopy, colonoscopy, ERCP, and endoscopic ultrasound. We had a 24 h duty call system to treat patients with GI bleeding and an ERCP duty call system for weekends to treat biliary pancreatitis. The following endoscopic facilities were available: endoscopic haemostasis methods including acute variceal band ligation and hemoclipps, polypectomy, mucosectomy, PEG, diagnostic and therapeutic endoscopic ultrasonography EUS, diagnostic ERCP, operative ERCP, such as papillotomy, septotomy, bile stone removal and lithotripsy, plastic and metal stenting, pancreatic stenting, endoscopic SO manometry, endoscopic drainage of the pancreatic pseudocysts, needle knife papillotomy, snare papillectomomy.
CLINICAL SKILLS, OPERATIONS, TECHNIQUES AND EXPERIENCE:
| Clinical skill, operation, technique, or type of experience | Number performed per year | Number performed in total | Years of experience |
|---|---|---|---|
| Abdominal ultrasound (diagnostic) | 200 | 5000 | 25 |
| Hepatobiliary scintigraphy (nuclear medicine) | 100 | 3000 | 30 |
| Upper GI endoscopy (gastroscopy) | 750 | 21000 | 28 |
| Colonoscopy | 1000 | 26000 | 26 |
| Polypectomy | 400 | 10400 | 26 |
| ERCP (total) | 300 | 6600 | 22 |
| NOTES (cystostomy, necrosectomy) | 10 | 150 | 15 |
| Endoscopic ultrasound (EUS) | 100 | 1500 | 15 |
| Endoscopic sphincter of Oddi manometry | 10 | 200 | 20 |
| Mucosectomy | 50 | 750 | 15 |
| ESD | 5 | 50 | 10 |
| EUS-FNA/FNB | 50 | 250 | 5 |
| POEM, G-POEM | 5 | 10 | 1 |
| EFTR | 5 | 5 | 1 |
| Capsule Endoscopy SB | 100 | 1500 | 15 |
| Capsule Endoscopy colon | 20 | 300 | 15 |
| Capsule Endoscopy gastric magnetic navigation | 300 | 900 | 3 |

MEDICAL REGISTRATION:
| Medical Council: | Registration Number: |
|---|---|
| Hungarian Medical Council | 45-326 |
| European Board of Gastroenterology (EUMS) | 1354 |
SPECIALIST TRAINING IN GASTROENTEROLOGY
| 1. Clinic and Hospital: First Department of Internal Medicine and Gastroenterology, University of Szeged Albert Szent-Györgyi Medical and Pharmaceutical Center |
|---|
| Training Director: Prof. Dr. László Csernay DMSc |
| Training Period From: 01.10.1988. To: 01.01.1990. |
| Position Held: clinical doctor |
| 2. Clinic and Hospital: Clinic and Hospital: First Department of Internal Medicine and Gastroenterology, University of Szeged Albert Szent-Györgyi Medical and Pharmaceutical Center |
| Training Director: Prof. Dr. Vince Varró DMSc |
| Training Period From: 01.01.1990. To: 01.01.1992. |
| Position Held: clinical doctor |
| 3. Clinic and Hospital: Clinic and Hospital: First Department of Internal Medicine and Gastroenterology, University of Szeged Albert Szent-Györgyi Medical and Pharmaceutical Center |
| Training Director: Prof. Dr. János Lonovics DMSc |
| Training Period From: 01.01.1992. To: 01.01.1994 |
| Position Held: Assistant of the Professor |
| 4. Clinic and Hospital: Sophia Hospital Zwolle and Academic Medical Center, Amsterdam, The Netherlands |
| Training Director: G. F. Nelis MD. PhD |
| Training Period From: 14.02.1994 To: 30.02.1994 |
| Position Held: Assistant of the Professor |
| 5. Clinic and Hospital: Hvidovre Hospital, Copenhagen, Denmark |
| Training Director: Prof. Dr. Peter Funch-Jensen DMSc |
| Training Period From: 01.09.1996 To: 01.06.1997 |
| Position Held: Assistant of the Professor |
| 6. Clinic and Hospital: Endoscopy Unit, Aarhus University Hospital, Aarhus, Denmark |
| Training Director: Prof. Aksel Kruse |
| Training Period From: 01.09.2020 To: 01.01.2021 |
| Position Held: Endoscopy Unit Director |
CURRENT PROFESSIONAL ACTIVITIES
| Clinical Activities: | |
|---|---|
| Institution: Bács-Kiskun County Municipality Hospital | |
| Present Position: Consultant and Scientific Advisor | Speciality: Gastroenterology, Endoscopy |
| Town: Kecskemét | Country: Hungary |
| Teaching Activities: | |
| Institution: First Department of Internal Medicine and Gastroenterology, University of Szeged Albert Szent-Györgyi Medical and Pharmaceutical Center | |
| Present Position: Professor of Medicine | Specialty: Gastroenterology, Internal Medicine |
| Town: Szeged | Country: Hungary |
| Research Activities: | |
| Institution: First Department of Internal Medicine and Gastroenterology, University of Szeged Albert Szent-Györgyi Medical and Pharmaceutical Center | |
| Present Position: Professor of Medicine | Specialty: PhD Doctoral School Leader |
| Town: Szeged | Country: Hungary |
Membership of Gastroenterology Societies (National/International):
| Member of the Executive Board Hungarian Society of Gastroenterology. 1996 - |
| Member of the Education Committee of the ESGE: 2008 - |
| Member of the European Association of Nuclear Medicine: 1997 - |
| Member of the International Gastro Surgical Club: 1995 - |
| President of the Endoscopy Session of the Hungarian Society of Gastroenterology 2008-2010, 2023 – 2025 (elected) |
ACADEMIC ACTIVITIES
| Books and chapters 22 |
| Number of Published Oral Presentations: 540 |
| International: 216 (with published abstracts) |
| Number of In Extenso Publications in Peer-Reviewed Journals: 72 |
| Citations: 573 |
| List of Publications: https://www.researchgate.net/profile/Laszlo-Madacsy |
Science Statistics
R.G. Score 39.37
Publications 309
Cumulative IF 76,610
H-Index 14
Sum of Citations 573
Patents
ColCap TM (endoscopic plastic cap for better polyp and adenoma detection)
Polypbrain TM (A.I. based polyp delineation, classification, and histological prediction website software) http://polypbrain.com/
Skills & Activities
| Skills | Endoscopic Retrograde Cholangiopancreatography, Endoscopic ultrasonography, Gastroscopy, Colonoscopy, Capsule Endoscopy, Magnetically controlled capsule endoscopy, Hepatobiliary Scintigraphy, Cholecystectomy, Acute Pancreatitis, Gastrointestinal Diseases, Pancreas, Hepatobiliary System, Biliary Tract Diseases, Pancreatic Diseases, Diagnostic Methods, EMR, ESD, Gastrointestinal Endoscopy, Endoscopic Sphincterotomy, Endoscopic Sphincter of Oddi Manometry, Electronic chromoendoscopy, Artificial Intelligence in Medicine |
| Languages | English, Hungarian |
| Scientific Memberships | Hungarian Society of Gastroenterology Governing Board Member of the Hungarian Society of Gastroenterology Endoscopy Section Hungarian Society of Gastroenterology Past President of Endoscopy Section Hungarian Society of Gastroenterology Board Member of Endoscopy Section Hungarian Society of Gastroenterology Elected President of Endoscopy Section Hungarian Society of Gastroenterology Board Member of Capsule Endoscopy Working Group of Endoscopy Section Hungarian Society of Gastroenterology Past Secretary of Motility Section Hungarian Society of Gastroenterology Board Member of Education Committee of ESGE Board Member of the Quality of Endoscopy Committee of ESGE |
| Scientific Interests | Gastrointestinal motility, functional gastrointestinal disorders, sphincter of Oddi dysfunction, biliary dyskinesia, endoscopic necrosectomy in pancreatitis, endoscopic submucosal dissection, capsule endoscopy, magnetically controlled capsule endoscopy, electronic chromoendoscopy, artificial intelligence in medicine and endoscopy |
PUBLICATIONS:
In Extenso Publications in international journals and books
1. Dubravcsik Z, Hritz I, Keczer B, Novák P, Lovász BD, Madácsy L.: Network meta-analysis of prophylactic pancreatic stents and non-steroidal anti-inflammatory drugs in the prevention of moderate-to-severe post-ERCP pancreatitis. Pancreatology 21 (4): 704-713, 2021 IF: 1.269
2. Gyökeres T., Madácsy L. (2020) Treatment of Acute Biliary Pancreatitis. In: Testoni P.A., Inoue H., Wallace M.B. (eds) Gastrointestinal and Pancreatico-Biliary Diseases: Advanced Diagnostic and Therapeutic Endoscopy. Springer, Cham. https://doi.org/10.1007/978-3-030-29964-4_91-1
3. Barbara Dorottya Lovász, Milán Szalai, László Oczella, Ádám Finta, Zsolt Dubravcsik & László Madácsy: Improved adenoma detection with linked color imaging technology compared to white-light colonoscopy, Scandinavian Journal of Gastroenterology, 55:7, 877-883, (2020) DOI: 10.1080/00365521.2020.1786850
IF: 0.799
4. Dubravcsik Z, Hritz I, Szepes A, Madácsy L.: Risk factors of post-ERCP pancreatitis in high-risk patients despite prevention with prophylactic pancreatic stents. Scandinavian Journal of Gastroenterology 55(1):1-5, 2019
IF: 0.799
5. Madácsy L, Kaltsidis H.: Endoscopic ultrasound-guided extraluminal drainage. Novel concepts, challenges and future directions, Gastrointest Interv 2017;6:122–129
6. Madacsy L, Dubravcsik Z and Szepes A.: Postcholecystectomy Syndrome: From Pathophysiology to Differential Diagnosis – A Critical Review. Pancreat Disord Ther 2015. nov. 19. 5:162. doi:10.4172/2165-7092.1000162
7. Bor R., Madácsy L., Fábián A., Szepes A., Szepes Z: Endoscopic retrograde pancreatography: When should we do it? World J Gastrointest Endosc. 2015 Aug 25;7(11):1023-31.
8. Dubravcsik Z, Szepes A, Hritz I, Madácsy L. Small-caliber rescue pancreatic stenting for severe post-ERCP pancreatitis: a useful tool to pull the pancreas out of the fire. Endoscopy. 2015 May;47(5):467-8. doi: 10.1055/s-0034-1391309.
IF: 5.634
9. Dubravcsik Z, Madácsy L, Gyökeres T, Vincze Á, Szepes Z, Hegyi P, Hritz I, Szepes A; Hungarian Pancreatic Study Group. Preventive pancreatic stents in the management of acute biliary pancreatitis (PREPAST trial): pre-study protocol for a multicenter, prospective, randomized, interventional, controlled trial. Pancreatology. 2015 Mar-Apr;15(2):115-23. doi: 10.1016/j.pan.2015.02.007.
IF: 2.406
10. Søfteland E, Brock C, Frøkjær JB, Brøgger J, Madácsy L, Gilja OH, Arendt-Nielsen L, Simrén M, Drewes AM, Dimcevski G. Association between visceral, cardiac and sensorimotor polyneuropathies in diabetes mellitus. J Diabetes Complications. 2014 May-Jun;28(3):370-7. doi: 10.1016
IF: 2.056
11. Dubravcsik Zs., Hritz I., Fejes R., Szepes A., Madácsy L.: Endoscopic Therapy of Refractory Post-Papillotomy Bleeding With Electrocautery Forceps Coagulation Method Combined With Prophylactic Pancreatic Stenting. Video Journal and Encyclopedia of GI Endoscopy January 2014, Pages 628-631
12. Hritz I, Fejes R, Székely A, Székely I, Horváth L, Sárkány A, Altorjay A, Madácsy L. Endoscopic transluminal pancreatic necrosectomy using a self-expanding metal stent and high-flow water-jet system. World J Gastroenterol. 2013 Jun 21;19(23):3685-92. doi: 10.3748
IF: 2.547
13. Dubravcsik Z, Hritz I, Fejes R, Balogh G, Viranyi Z, Hausinger P, Szekely A, Szepes A, Madácsy L: Early ERCP and biliary sphincterotomy with or without small-caliber pancreatic stent insertion in patients with acute biliary pancreatitis: better overall outcome with adequate pancreatic drainage. Scandinavian journal of gastroenterology 2012, 47(6):729-736.
IF: 2.019
14. Hritz I, Dubravcsik Z, Szepes A, Madácsy L: Does removal of prophylactic pancreatic stents induce acute pancreatitis? Gastrointestinal endoscopy 2011, 74(6):1429-1430 (Letter to the Editor); author reply 1430.
IF: 4.878
15. Kunwald P, Drewes AM, Kjaer D, Gravesen FH, McMahon BP, Madácsy L, Funch-Jensen P, Gregersen H: A new distensibility technique to measure sphincter of Oddi function. Neurogastroenterology and motility: the official journal of the European Gastrointestinal Motility Society 2010, 22(9):978-983, e253.
IF: 3.349
16. Fejes R, Kurucsai G, Szekely A, Szekely I, Altorjay A, Madácsy L: Feasibility and safety of emergency ERCP and small-caliber pancreatic stenting as a bridging procedure in patients with acute biliary pancreatitis but difficult sphincterotomy. Surgical endoscopy 2010, 24(8):1878-1885.
IF: 3.436
17. Altorjay A, Mucs M, Rull M, Tihanyi Z, Hamvas B, Madácsy L, Paal B: Recurrent, nonmalignant tracheoesophageal fistulas and the need for surgical improvisation. The Annals of thoracic surgery 2010, 89(6):1789-1796.
IF: 3.558
18. Fejes R, Kurucsai G, Székely A, Luka F, Altorjay Á, and Madácsy L: „Gallstone Ileus, Bouveret’s Syndrome and Choledocholithiasis in a Patient with Billroth II Gastrectomy – A Case Report of Combined Endoscopic and Surgical Therapy” Case Rep Gastroenterol. 2010, 4(1): 71–78.
19. Madácsy L, Kurucsai G, Joo I, Godi S, Fejes R, Szekely A: Rescue ERCP and insertion of a small-caliber pancreatic stent to prevent the evolution of severe post-ERCP pancreatitis: a case-controlled series. Surgical Endoscopy 2009, 23(8):1887-1893.
IF: 3.307
20. Madácsy L, Kurucsai G, Fejes R, Szekely A, Szekely I: Prophylactic pancreas stenting followed by needle-knife fistulotomy in patients with sphincter of Oddi dysfunction and difficult cannulation: new method to prevent post-ERCP pancreatitis. Digestive endoscopy : official journal of the Japan Gastroenterological Endoscopy Society 2009, 21(1):8-13.
IF: 0.333
21. Kurucsai G, Joo I, Fejes R, Szekely A, Szekely I, Tihanyi Z, Altorjay A, Funch-Jensen P, Varkonyi T, Madácsy L: Somatosensory hypersensitivity in the referred pain area in patients with chronic biliary pain and a sphincter of Oddi dysfunction: new aspects of an almost forgotten pathogenetic mechanism. The American Journal of Gastroenterology 2008, 103(11):2717-2725.
IF: 6.444
22. Madácsy L, Fejes R, Kurucsai G, Joo I, Szekely A, Bertalan V, Szepes A, Lonovics J: Characterization of functional biliary pain and dyspeptic symptoms in patients with sphincter of Oddi dysfunction: effect of papillotomy. World Journal of Gastroenterology : World journal of gastroenterology WJG 2006, 12(42):6850-6856.
23. Funch-Jensen P, Drewes AM, Madácsy L: Evaluation of the biliary tract in patients with functional biliary symptoms. World Journal of Gastroenterology : WJG 2006, 12(18):2839-2845.
24. Bertalan V, Szepes A, Lonovics J, Madácsy L: Assessment of the reproducibility of quantitative hepatobiliary scintigraphy (QHBS) in patients with sphincter of Oddi dysfunction (SOD)–inappropriate method or intermittent disease? Hepato-gastroenterology 2006, 53(68):160-165.
IF: 0.756
25. Szepes A, Bertalan V, Varkonyi T, Pavics L, Lonovics J, Madácsy L: Diagnosis of gallbladder dyskinesia by quantitative hepatobiliary scintigraphy. Clinical nuclear medicine 2005, 30(5):302-307.
IF: 1.800
26. Madácsy L, Szepes A, Nagy I, Velosy B, Tiszlavicz L, Pavics L, Csernay L, Lonovics J:Congenital hepatic fibrosis in a patient with suspected postcholecystectomy syndrome: hepatobiliary scintigraphy at diagnosis and during follow-up. Clinical nuclear medicine 2004, 29(1):55-59.
IF: 1.582
27. Madácsy L, Matzen P, Funch-Jensen P: Analysis of the motor function of the human sphincter of Oddi by endoscopic retrograde cinecholangiography gated by manometry–a report of a case. Hepato-gastroenterology 2004, 51(60):1619-1622.
IF: 0.696
28. Bertalan V, Madácsy L, Pavics L, Lonovics J: Scintigraphic sign of functional biliary obstruction is pathognomic for sphincter of Oddi dysfunction. Hepato- gastroenterology 2004, 51(55):76-81.
IF: 0.696
29. Madácsy L, Szepes A, Bertalan V, Funch-Jensen P: Is hepatobiliary scintigraphy insensitive for the diagnosis of sphincter of Oddi dysfunction? Gut 2003, 52(9):1385-1386. (Letter to the editor)
IF: 5.883
30. Madácsy L, Molnar T, Nagy I, Tiszlavicz L, Lonovics J: Recurrent nonvariceal upper gastrointestinal bleeding in a patient with gastroduodenal schistosomiasis. Endoscopy 2003, 35(3):230-233.
IF: 3.227
31. Madácsy L, Bertalan V, Szepes A, Lonovics J: Effect of nalbuphine on the motility of the sphincter of Oddi in patients with suspected sphincter of Oddi dysfunction. Gastrointestinal endoscopy 2003, 57(3):319-323.
IF: 3.328
32. Madácsy L, Velosy B, Szepes A, Szilvassy Z, Pavics L, Csernay L, Lonovics J: Effect of nitric oxide on gallbladder motility in patients with acalculous biliary pain: a cholescintigraphic study. Digestive diseases and sciences 2002, 47(9):1975-1981.
IF: 1.438
33. Madácsy L, Szepes A, Bertalan V, Paavics L, Csernay L, Lonovics J: Enhanced filling and cholecystokinin-induced emptying of the human gallbladder after glyceryl trinitrate administration: a scintigraphic sign of functional cystic duct syndrome. Clinical nuclear medicine 2002, 27(9):660-662.
IF: 0.502
34. Varkonyi TT, Lengyel C, Madácsy L, Velosy B, Kempler P, Fazekas T, Pavics L, Csernay L, Lonovics J: Gallbladder hypomotility in diabetic polyneuropathy. Clinical autonomic research: official journal of the Clinical Autonomic Research Society 2001, 11(6):377-381.
IF: 0.916
35. Madácsy L, Middelfart HV, Matzen P, Hojgaard L, Funch-Jensen P: Quantitative hepatobiliary scintigraphy and endoscopic sphincter of Oddi manometry in patients with suspected sphincter of Oddi dysfunction: assessment of flow-pressure relationship in the biliary tract. European journal of gastroenterology & hepatology 2000, 12(7):777-786.
IF: 1.1420
36. Madácsy L, Middelfart HV, Matzen P, Funch-Jensen P: Video manometry of the sphincter of Oddi: a new aid for interpreting manometric tracings and excluding manometric artefacts. Endoscopy 2000, 32(1):20-26.
IF: 1.8170
37. Velosy B, Madácsy L, Szepes A, Pavics L, Csernay L, Lonovics J: The effects of somatostatin and octreotide on the human sphincter of Oddi. European journal of gastroenterology & hepatology 1999, 11(8):897-901.
IF: 1.583
38. Madácsy L, Toftdahl DB, Middelfart HV, Hojgaard L, Funch-Jensen P: Comparison of the dynamics of bile emptying by quantitative hepatobiliary scintigraphy before and after cholecystectomy in patients with uncomplicated gallstone disease. Clinical nuclear medicine 1999, 24(9):649-654.
IF: 0.253
39. Lonovics J, Madácsy L, Szepes A, Szilvassy Z, Velosy B, Varro V: Humoral mechanisms and clinical aspects of biliary tract motility. Scandinavian journal of gastroenterology Supplement 1998, 228:73-89.
IF: 2.360
40. Velosy B, Madácsy L, Lonovics J, Csernay L: Effect of glyceryl trinitrate on the sphincter of Oddi spasm evoked by prostigmine-morphine administration. European journal of gastroenterology & hepatology 1997, 9(11):1109-1112.
IF: 1.453
41. Szilvassy Z, Nagy I, Madácsy L, Hajnal F, Velosy B, Takacs T, Lonovics J: Beneficial effect of lovastatin on sphincter of Oddi dyskinesia in hypercholesterolemia and hypertriglyceridemia. The American journal of gastroenterology 1997, 92(5):900-902.
IF: 2.344
42. Madácsy L, Velosy B, Lonovics J, Csernay L: Evaluation of results of the prostigmine-morphine test with quantitative hepatobiliary scintigraphy: a new method for the diagnosis of sphincter of Oddi dyskinesia. European journal of nuclear medicine 1995, 22(3):227-232.
IF: 2.930
43. Madácsy L, Velosy B, Lonovics J, Csernay L: Differentiation between organic stenosis and functional dyskinesia of the sphincter of Oddi with amyl nitrite-augmented quantitative hepatobiliary scintigraphy. European journal of nuclear medicine 1994, 21(3):203-208.
IF: 2.690